Rheumatoid arthritis (RA)
Rheumatoid arthritis (RA) is a multifaceted autoimmune disorder characterized by chronic inflammation primarily affecting the joints. This condition not only causes joint pain, swelling, and deformity but also extends beyond the musculoskeletal system to impact various organs and tissues in the body. While the exact cause of RA remains elusive, researchers believe it stems from a combination of genetic predisposition and environmental triggers^[1].
The Role of Inflammation in RA
At the core of rheumatoid arthritis is inflammation of the synovium, the membrane lining the joints. This inflammation prompts the formation of pannus—a thickened tissue that can erode cartilage and bone within the joint, leading to joint damage and deformity over time^[2]. The systemic nature of RA means that inflammation can also affect other parts of the body, causing fatigue, fever, and weight loss^[3].
Symptoms and Patterns of Joint Involvement
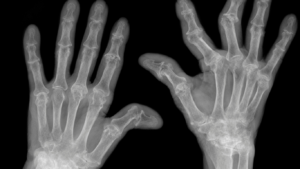
RA is characterized by a symmetrical pattern of joint involvement, typically affecting joints on both sides of the body simultaneously. Commonly affected areas include the hands (including wrists and fingers), knees, feet, and elbows. This symmetrical presentation distinguishes RA from other forms of arthritis, such as osteoarthritis, which may affect only one side of the body^[4].
Diagnosis and Assessment of RA
Diagnosing RA involves a comprehensive evaluation combining clinical assessments, blood tests, and imaging studies. Elevated levels of specific antibodies, such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP), are often detected in individuals with RA, aiding in the diagnosis^[5]. Imaging techniques like X-rays and magnetic resonance imaging (MRI) help visualize joint damage and assess disease severity.
Treatment Approaches for RA
The goals of RA treatment are to manage symptoms, prevent joint damage, and enhance quality of life. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, are pivotal in slowing disease progression by suppressing the immune response^[6]. Biologic agents, including tumor necrosis factor (TNF) inhibitors, target specific components of the immune system implicated in RA inflammation, revolutionizing treatment outcomes^[7].
Comprehensive Care and Lifestyle Adjustments
Beyond medication, physical therapy and occupational therapy are vital components of RA management. These therapies focus on improving joint function, mobility, and independence in daily activities. Embracing lifestyle modifications—such as regular exercise tailored to individual capabilities, a balanced diet rich in anti-inflammatory foods, and stress management techniques—can further optimize overall well-being and symptom control^[8].
Challenges and Coping Strategies
Living with RA poses unique challenges that can vary from person to person. Chronic pain, fatigue, and emotional distress associated with a long-term condition necessitate a holistic and personalized approach to care. Engaging in support groups and educational programs can offer valuable resources, emotional support, and a sense of community for individuals navigating the complexities of RA^[9].
Advancements in Research and Hope for the Future
While there is currently no cure for RA, ongoing research efforts continue to advance our understanding of its underlying mechanisms and develop more targeted therapies. The goal is to achieve better disease control and, ideally, remission for individuals living with RA. Promising advancements in immunology and personalized medicine hold hope for improving outcomes and enhancing the quality of life for those affected by this chronic autoimmune disorder^[10].
Read each of the 6 Rheumatoid Arthritis Subtypes.
6 Subtypes of Rheumatoid Arthritis
Juvenile Rheumatoid Arthritis (JRA): 2 of 6 Subtypes of Rheumatoid Arthritis (RA)
Juvenile Rheumatoid Vasculitis (JRV): 3 of 6 Subtypes of Rheumatoid Arthritis (RA)
Juvenile Palindromic Rheumatism: 4 of 6 Subtypes of Rheumatoid Arthritis (RA)
Juvenile Undifferentiated Connective Tissue Disease (UCTD): 5 of 6 Subtypes of Rheumatoid Arthritis (RA)
Juvenile Seropositive Rheumatoid Arthritis: 6 of 6 Subtypes of Rheumatoid Arthritis (RA)
And the Rheumatoid Arthritis Severity Scale
- Mayo Clinic. (2022). Rheumatoid arthritis. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
- Firestein, G. S. (2003). Evolving concepts of rheumatoid arthritis. Nature, 423(6937), 356-361. https://doi.org/10.1038/nature01661
- Scott, D. L., Wolfe, F., & Huizinga, T. W. (2010). Rheumatoid arthritis. The Lancet, 376(9746), 1094-1108. https://doi.org/10.1016/S0140-6736(10)60826-4
- Arthritis Foundation. (2022). Rheumatoid arthritis. https://www.arthritis.org/diseases/rheumatoid-arthritis
- American College of Rheumatology. (2010). Rheumatoid arthritis. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Rheumatoid-Arthritis
- Smolen, J. S., Landewé, R., Bijlsma, J., et al. (2020). EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Annals of the Rheumatic Diseases, 79(6), 685-699. https://doi.org/10.1136/annrheumdis-2019-216655
- McInnes, I. B., & Schett, G. (2011). The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365(23), 2205-2219. https://doi.org/10.1056/NEJMra1004965
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2022). Handout on health: Rheumatoid arthritis. https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
- Matcham, F., Scott, I. C., Rayner, L., et al. (2014). The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism, 44(2), 123-130. https://doi.org/10.1016/j.semarthrit.2014.05.001
- Smolen, J. S., Aletaha, D., McInnes, I. B., et al. (2016). Rheumatoid arthritis. The Lancet, 388(10055), 2023-2038. https://doi.org/10.1016/S0140-6736(16)30173-8