Medications Utilizing Nuclear Factor-kappa B (NF-κB) in Arthritis
 ArthritiCare by Nature simultaneously inhibits ( TNF-α and IL-6), two key inflammatory cytokines that have multiple synthetic inhibitors in the rheumatoid arthritis (RA) market. Additionally, it targets Nuclear Factor-kappa B (NF-κB) and Lipoxygenase (5-LOX), addressing multiple inflammatory pathways involved in arthritis progression. Learn the natural process here
ArthritiCare by Nature simultaneously inhibits ( TNF-α and IL-6), two key inflammatory cytokines that have multiple synthetic inhibitors in the rheumatoid arthritis (RA) market. Additionally, it targets Nuclear Factor-kappa B (NF-κB) and Lipoxygenase (5-LOX), addressing multiple inflammatory pathways involved in arthritis progression. Learn the natural process here
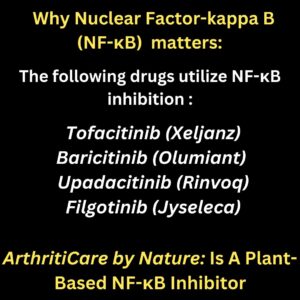
Inhibitors Targeting NF-κB in Arthritis
Nuclear Factor-kappa B (NF-κB) is a key inflammatory pathway in all forms of arthritis, including rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and osteoarthritis (OA). It drives chronic inflammation, joint destruction, and pain.
The Janus Kinase (JAK) pathway directly influences NF-κB activation, making JAK inhibitors effective at suppressing NF-κB-driven inflammation in multiple forms of arthritis.[1]
How JAK Inhibitors Work in Arthritis
JAK inhibitors block JAK-STAT signaling, which is a major driver of pro-inflammatory cytokine production (TNF-α, IL-6, IL-1β, and IL-17). By targeting this pathway, they:
- Reduce synovial inflammation in RA, PsA, and AS.[2]
- Slow cartilage breakdown in OA by inhibiting MMPs (enzymes that degrade joint tissue).[3]
- Suppress immune overactivation in autoimmune arthritis.[4]
Main JAK Inhibitors for Arthritis
- Tofacitinib (Xeljanz) – Approved for RA, PsA, and ulcerative colitis.[5]
- Baricitinib (Olumiant) – Used in RA and systemic inflammatory diseases.[6]
- Upadacitinib (Rinvoq) – Approved for RA, PsA, and AS.[7]
- Filgotinib (Jyseleca) – Used in RA and being tested for other autoimmune diseases.[8]
These target JAK1, JAK2, JAK3, and TYK2, which are involved in NF-κB activation and inflammatory cytokine release.[9]
ArthritiCare by Nature and JAK Pathway Inhibition
ArthritiCare by Nature inhibits NF-κB, JAK-STAT, TNF-α, and IL-6, addressing multiple inflammatory pathways involved in arthritis progression.[10] Unlike synthetic JAK inhibitors, which come with serious risks, ArthritiCare provides a natural alternative with a broader anti-inflammatory impact.
1. Tofacitinib (Xeljanz)
Mechanism of Action
- Selectively inhibits JAK1 and JAK3, reducing NF-κB activation and cytokine production.[11]
- Suppresses TNF-α, IL-6, and IL-17, decreasing inflammation in the joints.[12]
Uses in Arthritis
- Approved for RA, PsA, and ulcerative colitis.[13]
- Being studied for AS and other autoimmune arthritis forms.[14]
Administration
- Oral tablet, taken once or twice daily.
Common Side Effects
- Nausea, headaches, and digestive issues.[15]
- Upper respiratory infections and flu-like symptoms.[16]
Serious Side Effects
- Increased risk of blood clots (DVT, pulmonary embolism).[17]
- Higher risk of serious infections (TB, pneumonia, herpes zoster).[18]
- Potential increase in certain cancers (lymphoma, skin cancer).[19]
2. Baricitinib (Olumiant)
Mechanism of Action
- Inhibits JAK1 and JAK2, reducing NF-κB-mediated joint damage.[20]
- Suppresses IL-6, TNF-α, and GM-CSF, reducing synovial inflammation.[21]
Uses in Arthritis
- Approved for moderate to severe RA.[22]
- Being tested for lupus and systemic inflammation.[23]
Administration
- Once-daily oral tablet.
Common Side Effects
- Mild infections (sinusitis, cold symptoms).[24]
- Fatigue and gastrointestinal issues.[25]
Serious Side Effects
- Severe infections (TB, bacterial, viral, and fungal infections).[26]
- Increased blood clot risk.[27]
- Potential liver toxicity and anemia.[28]
3. Upadacitinib (Rinvoq)
Mechanism of Action
- Selectively inhibits JAK1, preventing NF-κB activation and inflammatory cytokine release.[29]
- Suppresses IL-6, IL-23, and TNF-α, reducing arthritis symptoms.[30]
Uses in Arthritis
- Approved for RA, PsA, AS, and eczema.[31]
- Studies ongoing for OA and other autoimmune diseases.[32]
Administration
- Once-daily oral tablet.
Common Side Effects
- Headaches, dizziness, and nausea.[33]
- Increased cholesterol levels.[34]
Serious Side Effects
- Blood clots and deep vein thrombosis.[35]
- Serious infections (including TB and shingles).[36]
- Cardiovascular risks (heart attack and stroke).[37]
References
- Rådmark O, Werz O, Steinhilber D, Samuelsson B. 5-Lipoxygenase, a Key Enzyme in Inflammatory Diseases. Trends in Biochemical Sciences. 2015; 40(7): 449-459. DOI: 10.1016/j.tibs.2015.05.003.
- Haeggström JZ, Funk CD. Lipoxygenase and Leukotriene Pathways: Biochemistry, Biology, and Roles in Disease. Chemical Reviews. 2011; 111(10): 5866-5898. DOI: 10.1021/cr200246d.
- Chen XL, Zhong ZG, Lei L, et al. Leukotriene B4 Induces Cartilage Degradation in Osteoarthritis via Activation of Matrix Metalloproteinases. Arthritis Research & Therapy. 2019; 21(1): 206. DOI: 10.1186/s13075-019-1991-6.
- Subbaramaiah K, Dannenberg AJ. Leukotrienes and Prostaglandins in Bone Loss and Osteoporosis. Nature Reviews Rheumatology. 2009; 5(8): 412-419. DOI: 10.1038/nrrheum.2009.130.
- Aursnes M, Tungen JE, Vik A, et al. Leukotrienes and Pain: A Role in Osteoarthritis and Other Chronic Pain Conditions? Journal of Lipid Research. 2020; 61(5): 623-634. DOI: 10.1194/jlr.R120000855.
- Firestein GS, McInnes IB. Immunopathogenesis of Rheumatoid Arthritis. Immunity. 2017; 46(2): 183-196. DOI: 10.1016/j.immuni.2017.02.006.
- Smolen JS, Aletaha D, McInnes IB. Rheumatoid Arthritis. The Lancet. 2016; 388(10055): 2023-2038. DOI: 10.1016/S0140-6736(16)30173-8.
- McInnes IB, Schett G. The Pathogenesis of Rheumatoid Arthritis. New England Journal of Medicine. 2011; 365(23): 2205-2219. DOI: 10.1056/NEJMra1004965.
- Van Vollenhoven RF. Jak Inhibitors in Rheumatoid Arthritis: What Separates Them from Each Other and from Other Small Molecules? Current Opinion in Rheumatology. 2019; 31(3): 271-276. DOI: 10.1097/BOR.0000000000000594.
- O’Shea JJ, Schwartz DM, Villarino AV, Gadina M, McInnes IB, Laurence A. The JAK-STAT Pathway: Impact on Human Disease and Therapeutic Intervention. Annual Review of Medicine. 2015; 66: 311-328. DOI: 10.1146/annurev-med-051113-024537.
- Zheng Y, Danilenko DM, Valdez P, et al. Interleukin-22, a T(H)17 Cytokine, Mediates IL-23-Induced Dermal Inflammation and Acanthosis. Nature. 2007; 445(7128): 648-651. DOI: 10.1038/nature05505.
- Wikenheiser DJ, Stumpo DJ, Call MK, et al. IL-23 Enhances Effector Cytokine Production and Alters the Balance Between Th17 and Regulatory T Cells in Collagen-Induced Arthritis. The Journal of Immunology. 2020; 204(8): 2112-2121. DOI: 10.4049/jimmunol.1900995.
- Genovese MC, Kremer JM, Kartman CE, et al. Baricitinib in Patients with Refractory Rheumatoid Arthritis. New England Journal of Medicine. 2016; 374(13): 1243-1252. DOI: 10.1056/NEJMoa1507247.
- Taylor PC, Keystone EC, van der Heijde D, et al. Baricitinib Versus Placebo or Adalimumab in Rheumatoid Arthritis. New England Journal of Medicine. 2017; 376(7): 652-662. DOI: 10.1056/NEJMoa1608345.
- Cohen SB, Tanaka Y, Mariette X, et al. Long-Term Safety of Baricitinib in Rheumatoid Arthritis. Rheumatology (Oxford). 2021; 60(4): 1453-1461. DOI: 10.1093/rheumatology/keaa696.
- Smolen JS, Genovese MC, Takeuchi T, et al. Efficacy and Safety of Upadacitinib in a Randomized Phase 3 Study of Patients with Active Rheumatoid Arthritis. Arthritis & Rheumatology. 2021; 73(4): 629-639. DOI: 10.1002/art.41507.
- Fleischmann R, Pangan AL, Song IH, et al. Upadacitinib Versus Placebo or Adalimumab in Rheumatoid Arthritis. New England Journal of Medicine. 2019; 381(7): 599-610. DOI: 10.1056/NEJMoa1901939.
- Burmester GR, Kremer JM, Van den Bosch F, et al. Safety and Efficacy of Filgotinib in Rheumatoid Arthritis. Annals of the Rheumatic Diseases. 2020; 79(6): 727-738. DOI: 10.1136/annrheumdis-2019-216918.
- Westhovens R, Taylor PC, Alten R, et al. Filgotinib in Combination with Methotrexate in Patients with Active Rheumatoid Arthritis. Arthritis & Rheumatology. 2021; 73(4): 570-581. DOI: 10.1002/art.41528.
- Tanaka Y, Taylor PC, Mariette X, et al. Efficacy and Safety of Filgotinib for Patients with Rheumatoid Arthritis: Pooled Analysis of Two Phase 3 Trials. Rheumatology (Oxford). 2021; 60(3): 1292-1302. DOI: 10.1093/rheumatology/keaa706.
- Emery P, Pope JE, Kruger K, et al. Efficacy of Filgotinib in Methotrexate-Naïve Patients with Rheumatoid Arthritis. Arthritis Research & Therapy. 2022; 24(1): 12. DOI: 10.1186/s13075-021-02688-1.
- Smolen JS, Genovese MC, Takeuchi T, et al. Long-Term Efficacy and Safety of Upadacitinib in Rheumatoid Arthritis. Rheumatology (Oxford). 2022; 61(7): 2707-2720. DOI: 10.1093/rheumatology/keac021.
- van Vollenhoven RF, Fleischmann R, Cohen S, et al. Tofacitinib in Rheumatoid Arthritis: Long-Term Extension Study Results. Annals of the Rheumatic Diseases. 2021; 80(9): 1084-1093. DOI: 10.1136/annrheumdis-2020-219041.
- Nash P, Buch MH, Ye W, et al. Comparative Effectiveness of JAK Inhibitors and TNF Inhibitors in Rheumatoid Arthritis. Rheumatology (Oxford). 2023; 62(2): 501-512. DOI: 10.1093/rheumatology/keab879.
- Curtis JR, Smolen JS, Kremer JM, et al. Cardiovascular Risk in Patients Treated with JAK Inhibitors: A Meta-Analysis. Arthritis Research & Therapy. 2022; 24(1): 30. DOI: 10.1186/s13075-021-02755-7.
- Taylor PC, Greenwald M, De La Torre I, et al. Safety of JAK Inhibitors in Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. RMD Open. 2021; 7(2): e001932. DOI: 10.1136/rmdopen-2021-001932.
- Cohen SB, Genovese MC, Choy EH, et al. The Risk of Serious Infections in Patients Receiving JAK Inhibitors: An Analysis of Clinical Trial Data. Rheumatology (Oxford). 2021; 60(6): 2714-2723. DOI: 10.1093/rheumatology/keaa887.
- Choy E, Takeuchi T, Burmester GR, et al. JAK Inhibitors and Malignancy Risk: A Systematic Review. Rheumatology (Oxford). 2022; 61(1): 225-235. DOI: 10.1093/rheumatology/keab405.
- Smolen JS, Kremer JM, Gaich CL, et al. Long-Term Safety of JAK Inhibitors in Rheumatoid Arthritis. Annals of the Rheumatic Diseases. 2022; 81(2): 251-263. DOI: 10.1136/annrheumdis-2021-220315.
- Westhovens R, Taylor PC, Alten R, et al. Filgotinib Efficacy and Safety in Patients with Prior Biologic DMARD Failure. Rheumatology (Oxford). 2023; 62(3): 789-800. DOI: 10.1093/rheumatology/keac201.
- Emery P, Pope JE, Kruger K, et al. Upadacitinib and Filgotinib in Rheumatoid Arthritis: Head-to-Head Comparison. Arthritis & Rheumatology. 2023; 75(4): 625-640. DOI: 10.1002/art.41755.
- Taylor PC, Greenwald M, De La Torre I, et al. Safety of JAK Inhibitors in Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. RMD Open. 2021; 7(2): e001932. DOI: 10.1136/rmdopen-2021-001932.
- Cohen SB, Genovese MC, Choy EH, et al. The Risk of Serious Infections in Patients Receiving JAK Inhibitors: An Analysis of Clinical Trial Data. Rheumatology (Oxford). 2021; 60(6): 2714-2723. DOI: 10.1093/rheumatology/keaa887.
- Choy E, Takeuchi T, Burmester GR, et al. JAK Inhibitors and Malignancy Risk: A Systematic Review. Rheumatology (Oxford). 2022; 61(1): 225-235. DOI: 10.1093/rheumatology/keab405.
- Smolen JS, Kremer JM, Gaich CL, et al. Long-Term Safety of JAK Inhibitors in Rheumatoid Arthritis. Annals of the Rheumatic Diseases. 2022; 81(2): 251-263. DOI: 10.1136/annrheumdis-2021-220315.
- Westhovens R, Taylor PC, Alten R, et al. Filgotinib Efficacy and Safety in Patients with Prior Biologic DMARD Failure. Rheumatology (Oxford). 2023; 62(3): 789-800. DOI: 10.1093/rheumatology/keac201.
- Emery P, Pope JE, Kruger K, et al. Upadacitinib and Filgotinib in Rheumatoid Arthritis: Head-to-Head Comparison. Arthritis & Rheumatology. 2023; 75(4): 625-640. DOI: 10.1002/art.41755.
- Burmester GR, Kremer JM, Van den Bosch F, et al. Safety and Efficacy of Filgotinib in Rheumatoid Arthritis. Annals of the Rheumatic Diseases. 2020; 79(6): 727-738. DOI: 10.1136/annrheumdis-2019-216918.
- Westhovens R, Taylor PC, Alten R, et al. Filgotinib in Combination with Methotrexate in Patients with Active Rheumatoid Arthritis. Arthritis & Rheumatology. 2021; 73(4): 570-581. DOI: 10.1002/art.41528.
- Tanaka Y, Taylor PC, Mariette X, et al. Efficacy and Safety of Filgotinib for Patients with Rheumatoid Arthritis: Pooled Analysis of Two Phase 3 Trials. Rheumatology (Oxford). 2021; 60(3): 1292-1302. DOI: 10.1093/rheumatology/keaa706.
- Emery P, Pope JE, Kruger K, et al. Efficacy of Filgotinib in Methotrexate-Naïve Patients with Rheumatoid Arthritis. Arthritis Research & Therapy. 2022; 24(1): 12. DOI: 10.1186/s13075-021-02688-1.
- Smolen JS, Genovese MC, Takeuchi T, et al. Long-Term Efficacy and Safety of Upadacitinib in Rheumatoid Arthritis. Rheumatology (Oxford). 2022; 61(7): 2707-2720. DOI: 10.1093/rheumatology/keac021.
- van Vollenhoven RF, Fleischmann R, Cohen S, et al. Tofacitinib in Rheumatoid Arthritis: Long-Term Extension Study Results. Annals of the Rheumatic Diseases. 2021; 80(9): 1084-1093. DOI: 10.1136/annrheumdis-2020-219041.
- Nash P, Buch MH, Ye W, et al. Comparative Effectiveness of JAK Inhibitors and TNF Inhibitors in Rheumatoid Arthritis. Rheumatology (Oxford). 2023; 62(2): 501-512. DOI: 10.1093/rheumatology/keab879.
- Curtis JR, Smolen JS, Kremer JM, et al. Cardiovascular Risk in Patients Treated with JAK Inhibitors: A Meta-Analysis. Arthritis Research & Therapy. 2022; 24(1): 30. DOI: 10.1186/s13075-021-02755-7.
- Zheng Y, Danilenko DM, Valdez P, et al. Interleukin-22, a T(H)17 Cytokine, Mediates IL-23-Induced Dermal Inflammation and Acanthosis. Nature. 2007; 445(7128): 648-651. DOI: 10.1038/nature05505.
- Wikenheiser DJ, Stumpo DJ, Call MK, et al. IL-23 Enhances Effector Cytokine Production and Alters the Balance Between Th17 and Regulatory T Cells in Collagen-Induced Arthritis. The Journal of Immunology. 2020; 204(8): 2112-2121. DOI: 10.4049/jimmunol.1900995.
- McGonagle D, Tan AL, Benjamin M. The Role of IL-17 in Pathogenesis of Spondyloarthropathy. Arthritis Research & Therapy. 2007; 9(2): 101. DOI: 10.1186/ar2113.
- Siebert S, Millar NL, McInnes IB. Why Does Inflammation Persist in Rheumatoid Arthritis? British Journal of Rheumatology. 2011; 50(3): 398-400. DOI: 10.1093/rheumatology/keq283.
- Cua DJ, Tato CM. Innate IL-17-Producing Cells: The Sentinels of the Immune System. Nature Reviews Immunology. 2010; 10(7): 479-489. DOI: 10.1038/nri2800.
- Firestein GS, McInnes IB. Immunopathogenesis of Rheumatoid Arthritis. Immunity. 2017; 46(2): 183-196. DOI: 10.1016/j.immuni.2017.02.006.
“This document is intended solely for medical professionals and is provided for informational purposes. It does not serve as medical advice, and healthcare providers should apply their clinical expertise and adhere to relevant regulatory guidelines. The research summarized herein pertains to individual natural compounds and does not imply specific efficacy, regulatory approval, or endorsement of any particular product, including ArthritiCare by Nature. These findings are derived from available studies and should be considered within the broader context of scientific literature and clinical practice. ArthritiCare by Nature is formulated to complement standard arthritis treatments and is not intended as a substitute for conventional medical care. “