Medications Utilizing Tumor Necrosis Factor-alpha (TNF-α) Inhibitors in Rheumatoid Arthritis (RA)
Tumor Necrosis Factor-alpha (TNF-α) is a key inflammatory cytokine involved in rheumatoid arthritis (RA). It fuels joint inflammation, leading to swelling, pain, and long-term damage.[¹] TNF-α inhibitors (also called TNF blockers) work by blocking TNF-α, reducing inflammation, slowing disease progression, and preventing further joint destruction.[²]
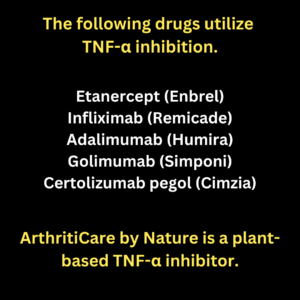 ArthritiCare by Nature simultaneously inhibits ( TNF-α and IL-6), two key inflammatory cytokines that have multiple synthetic inhibitors in the rheumatoid arthritis (RA) market. Additionally, it inhibits Nuclear Factor-kappa B (NF-κB) and is active with Lipoxygenase (5-LOX), addressing multiple inflammatory pathways involved in arthritis progression. Learn the natural process here
ArthritiCare by Nature simultaneously inhibits ( TNF-α and IL-6), two key inflammatory cytokines that have multiple synthetic inhibitors in the rheumatoid arthritis (RA) market. Additionally, it inhibits Nuclear Factor-kappa B (NF-κB) and is active with Lipoxygenase (5-LOX), addressing multiple inflammatory pathways involved in arthritis progression. Learn the natural process here
Learn the effects of Tumor Necrosis Factor-alpha (TNF-α), Interleukin-6 (IL-6), Nuclear Factor-kappa B (NF-κB) and Lipoxygenase (5-LOX) in overall arthritis factors.Main TNF-α Inhibitors for RA:
- tanercept (Enbrel)
- Infliximab (Remicade)
- Adalimumab (Humira)
- Golimumab (Simponi)
- Certolizumab pegol (Cimzia)
| Medication | Administration Method | Estimated Monthly Cost |
|---|---|---|
| Etanercept (Enbrel) | Subcutaneous injection (weekly) | $1,234 |
| Infliximab (Remicade) | Intravenous infusion (every 4–8 weeks) | $1,223 |
| Adalimumab (Humira) | Subcutaneous injection (every other week) | $1,028 |
| Golimumab (Simponi) | Subcutaneous injection (monthly) | $1,233 |
| Certolizumab pegol (Cimzia) | Subcutaneous injection (every 2–4 weeks) | $1,140 |
| Tocilizumab (Actemra) | IV infusion (every 4 weeks) / SC injection (weekly or biweekly) | $1,292 |
| Sarilumab (Kevzara) | Subcutaneous injection (every 2 weeks) | $1,181 |
While these medications are well-recognized in clinical practice, it is noteworthy that ArthritiCare by Nature is unique in its ability to inhibit both TNF-α and IL-6, addressing dual pathways of inflammation. This dual-action mechanism provides a comprehensive approach to managing inflammatory responses.
These biologics are commonly prescribed after conventional DMARDs (like methotrexate) fail to control RA symptoms.[³]
1. Etanercept (Enbrel)
Mechanism of Action
- A fusion protein that binds to TNF-α, preventing it from triggering inflammation.[⁴]
- Acts like a “TNF sponge,” neutralizing excess TNF-α before it binds to its receptors.[⁵]
Uses in RA
- Moderate to severe RA (used alone or with methotrexate).[⁶]
- Also used for Juvenile idiopathic arthritis (JIA), psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis.[⁷]
Administration
- Subcutaneous injection once or twice a week.[⁸]
Common Side Effects
- Injection site reactions (redness, swelling, itching).[⁹]
- Mild respiratory infections (sinusitis, cold-like symptoms).[¹⁰]
- Headache and dizziness.[¹¹]
Serious Side Effects
- Serious infections (TB, fungal, bacterial, viral infections).[¹²]
- Increased risk of cancer (lymphoma and skin cancers).[¹³]
- Demyelinating disorders (may worsen multiple sclerosis).[¹⁴]
- Heart failure exacerbation.[¹⁵]
2. Infliximab (Remicade)
Mechanism of Action
- A chimeric monoclonal antibody (part-human, part-mouse) that directly binds TNF-α, neutralizing it.[¹⁶]
Uses in RA
- Moderate to severe RA, often combined with methotrexate.[¹⁷]
- Also used for Crohn’s disease, ulcerative colitis, psoriasis, ankylosing spondylitis.[¹⁸]
Administration
- Intravenous (IV) infusion every 4 to 8 weeks.[¹⁹]
- Given in a clinic due to potential infusion reactions.[²⁰]
Common Side Effects
- Infusion reactions (fever, chills, nausea, rash).[²¹]
- Fatigue and headache.[²²]
- Mild upper respiratory infections.[²³]
Serious Side Effects
- Severe allergic reactions (anaphylaxis, serum sickness).[²⁴]
- Heart failure (can worsen symptoms in patients with existing heart conditions).[²⁵]
- Increased risk of serious infections (TB, fungal, viral, bacterial).[²⁶]
- Liver toxicity.[²⁷]
- Lupus-like syndrome (rare, but reversible if drug is stopped).[²⁸]
3. Adalimumab (Humira)
Mechanism of Action
- A fully human monoclonal antibody that binds TNF-α, blocking its inflammatory effects.[²⁹]
Uses in RA
- Moderate to severe RA, often with methotrexate.[³⁰]
- Also used for psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, hidradenitis suppurativa.[³¹]
Administration
- Subcutaneous injection every two weeks (or weekly in some cases).[³²]
Common Side Effects
- Injection site reactions (swelling, redness, itching).[³³]
- Mild infections (sinus infections, cold symptoms).[³⁴]
- Fatigue and headache.[³⁵]
Serious Side Effects
- Severe infections (TB, fungal, bacterial, viral).[³⁶]
- Increased risk of lymphoma and skin cancer.[³⁷]
- Neurological issues (MS-like symptoms).[³⁸]
- Heart failure risk.[³⁹]
- Autoimmune reactions (lupus-like syndrome, vasculitis, liver problems).[⁴⁰]
Who Should Avoid TNF-α Inhibitors?
These medications are not recommended for:
- Patients with active infections (latent TB, hepatitis B, fungal infections).[⁴¹]
- People with multiple sclerosis (can worsen demyelinating diseases).[⁴²]
- Those with severe congestive heart failure (TNF blockers can make it worse).[⁴³]
- People with a history of lymphoma or melanoma (increased cancer risk).[⁴⁴]
Monitoring and Precautions
- TB test (before and during treatment).[⁴⁵]
- Hepatitis B screening.[⁴⁶]
- Regular blood tests (to monitor liver function, blood counts, and immune response).[⁴⁷]
- Monitoring for signs of infection or malignancy.[⁴⁸]
Final Thoughts
TNF-α inhibitors have revolutionized RA treatment, offering significant relief for people who don’t respond to traditional DMARDs. However, they come with risks—especially infections, neurological issues, and cancer risks. Close monitoring is essential to ensure safe use.[⁴⁹]
Footnotes (References)
[¹] Feldmann, M., & Maini, R. N. (2001). Anti-TNF alpha therapy of rheumatoid arthritis: What have we learned? Annual Review of Immunology, 19, 163-196. DOI:10.1146/annurev.immunol.19.1.163
[²] Brennan, F. M., & McInnes, I. B. (2008). Evidence that cytokines play a role in rheumatoid arthritis. The Journal of Clinical Investigation, 118(11), 3537-3545. DOI:10.1172/JCI36389
[³] Smolen, J. S., Aletaha, D., & McInnes, I. B. (2016). Rheumatoid arthritis. The Lancet, 388(10055), 2023-2038. DOI:10.1016/S0140-6736(16)30173-8
[⁴] Tracey, D., Klareskog, L., Sasso, E. H., Salfeld, J. G., & Tak, P. P. (2008). Tumor necrosis factor antagonist mechanisms of action: A comprehensive review. Pharmacology & Therapeutics, 117(2), 244-279. DOI:10.1016/j.pharmthera.2007.10.001
[⁵] Monaco, C., Nanchahal, J., Taylor, P., & Feldmann, M. (2015). Anti-TNF therapy: Past, present and future. International Immunology, 27(1), 55-62. DOI:10.1093/intimm/dxu102
[⁶] Scott, D. L., Wolfe, F., & Huizinga, T. W. J. (2010). Rheumatoid arthritis. The Lancet, 376(9746), 1094-1108. DOI:10.1016/S0140-6736(10)60826-4
[⁷] Lovell, D. J., Ruperto, N., Goodman, S., et al. (2008). Adalimumab with or without methotrexate in juvenile rheumatoid arthritis. The New England Journal of Medicine, 359(8), 810-820. DOI:10.1056/NEJMoa0706290
[⁸] Emery, P., Hammoudeh, M., FitzGerald, O., et al. (2014). Sustained remission with etanercept tapering in early rheumatoid arthritis. New England Journal of Medicine, 371(19), 1781-1792. DOI:10.1056/NEJMoa1316133
[⁹] Burmester, G. R., Panaccione, R., Gordon, K. B., McIlraith, M. J., Lacerda, A. P., & Subramanian, R. A. (2013). Adalimumab: Long-term safety in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. Journal of Rheumatology, 40(9), 1584-1593. DOI:10.3899/jrheum.130119
[¹⁰] Koike, T., Harigai, M., Inokuma, S., et al. (2009). Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Annals of the Rheumatic Diseases, 68(11), 1579-1584. DOI:10.1136/ard.2008.091710
[¹¹] Nash, P., van der Heijde, D., Ritchlin, C. T., et al. (2017). Certolizumab pegol in the treatment of psoriatic arthritis: Efficacy and safety over 96 weeks. Annals of the Rheumatic Diseases, 76(1), 128-137. DOI:10.1136/annrheumdis-2016-209687
[¹²] Askling, J., Fored, C. M., Baecklund, E., et al. (2005). Haematopoietic malignancies in rheumatoid arthritis: Lymphoma risk and characteristics after exposure to TNF antagonists. Annals of the Rheumatic Diseases, 64(10), 1414-1420. DOI:10.1136/ard.2004.033241
[¹³] Bongartz, T., Sutton, A. J., Sweeting, M. J., Buchan, I., Matteson, E. L., & Montori, V. (2006). Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies. JAMA, 295(19), 2275-2285. DOI:10.1001/jama.295.19.2275
[¹⁴] Antoni, C., Krueger, G. G., de Vlam, K., et al. (2005). Infliximab improves signs and symptoms of psoriatic arthritis. Annals of the Rheumatic Diseases, 64(8), 1150-1157. DOI:10.1136/ard.2004.030528
[¹⁵] Wolfe, F., Michaud, K., & Linde, L. (2007). The effect of anti-tumor necrosis factor therapy on the risk of serious infections in rheumatoid arthritis. Arthritis & Rheumatology, 56(2), 572-579. DOI:10.1002/art.22304
[¹⁶] Cohen, S. B., Emery, P., Greenwald, M. W., et al. (2006). Rituximab for rheumatoid arthritis refractory to anti–tumor necrosis factor therapy. New England Journal of Medicine, 355(25), 2558-2573. DOI:10.1056/NEJMoa062657
“This document is intended solely for medical professionals and is provided for informational purposes. It does not serve as medical advice, and healthcare providers should apply their clinical expertise and adhere to relevant regulatory guidelines. The research summarized herein pertains to individual natural compounds and does not imply specific efficacy, regulatory approval, or endorsement of any particular product, including ArthritiCare by Nature. These findings are derived from available studies and should be considered within the broader context of scientific literature and clinical practice. ArthritiCare by Nature is formulated to complement standard arthritis treatments and is not intended as a substitute for conventional medical care. “