For Doctors and Rheumatoid Professionals Only
 List below are the effects of Tumor Necrosis Factor-alpha (TNF-α), Interleukin-6 (IL-6), Nuclear Factor-kappa B (NF-κB) and Lipoxygenase (5-LOX) in overall arthritis factors.
List below are the effects of Tumor Necrosis Factor-alpha (TNF-α), Interleukin-6 (IL-6), Nuclear Factor-kappa B (NF-κB) and Lipoxygenase (5-LOX) in overall arthritis factors.
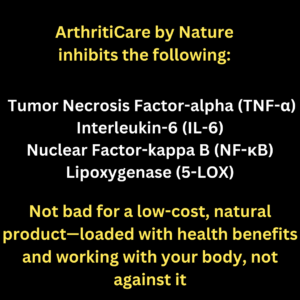
ArthritiCare by Nature simultaneously inhibits (TNF-α and IL-6), two key inflammatory cytokines that have multiple synthetic inhibitors in the rheumatoid arthritis (RA) market. Additionally, it targets Nuclear Factor-kappa B (NF-κB) and Lipoxygenase (5-LOX), addressing multiple inflammatory pathways involved in arthritis progression. Learn the natural process here
Here’s a detailed breakdown of TNF-α effects in Arthritis, with footnotes
1 Effects of Tumor Necrosis Factor-alpha (TNF-α) in Arthritis
TNF-α is a pro-inflammatory cytokine that plays a central role in autoimmune and inflammatory arthritis. It contributes to joint inflammation, cartilage degradation, bone erosion, and systemic complications in multiple forms of arthritis.
Many synthetic medications have been developed to block the TNF-α receptor, but they often come with significant side effects, such as immunosuppression, increased infection risk, and cardiovascular issues.1. Triggers Joint Inflammation by Activating Immune Responses
TNF-α stimulates synovial fibroblasts, macrophages, and dendritic cells, leading to increased production of inflammatory cytokines (IL-1, IL-6) and chemokines, fueling chronic inflammation and joint swelling.
- In RA and PsA, TNF-α induces persistent synovial inflammation, worsening joint pain and stiffness.[1]
- In OA, TNF-α contributes to low-grade chronic inflammation, accelerating cartilage degradation.[1]
- In AS, TNF-α drives inflammation in the spine and sacroiliac joints, leading to pain and stiffness.[1]
2. Leads to Cartilage Destruction by Stimulating Enzymes That Degrade Joint Tissue
TNF-α upregulates matrix metalloproteinases (MMPs), enzymes that break down collagen and proteoglycans, leading to irreversible cartilage damage.
- In RA and PsA, TNF-α fuels aggressive cartilage erosion, worsening joint deformities.[2]
- In OA, TNF-α accelerates cartilage thinning, contributing to the development of bone spurs (osteophytes).[2]
- In AS, TNF-α disrupts cartilage integrity in the spine, contributing to structural abnormalities.[2]
3. Causes Swelling and Pain by Increasing Blood Vessel Permeability
TNF-α induces vascular endothelial growth factor (VEGF), increasing capillary permeability, leading to fluid leakage, joint swelling, and tenderness.
- In RA and PsA, this results in severe synovitis, causing chronic joint pain and inflammation.[3]
- In OA, low-level TNF-α contributes to joint effusion (fluid buildup) and mild swelling.[3]
- In AS, vascular inflammation in spinal joints leads to swelling and restricted movement.[3]
4. Worsens Bone Loss by Promoting Osteoclast Activity
TNF-α stimulates RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand), a key regulator of osteoclast differentiation, leading to excessive bone resorption and joint destruction.
- In RA and PsA, TNF-α accelerates bone erosion, increasing the risk of joint deformities and osteoporosis.[4]
- In AS, TNF-α drives bone remodeling, contributing to spinal fusion and syndesmophyte formation.[4]
- In OA, TNF-α disrupts subchondral bone homeostasis, leading to sclerosis and joint instability.[4]
5. Can Lead to Systemic Effects Like Fatigue, Weight Loss, and Increased Risk of Heart Disease
Chronic TNF-α elevation contributes to fatigue, muscle wasting, and metabolic dysregulation, increasing cardiovascular risks.
- Fatigue and cachexia: TNF-α triggers metabolic abnormalities, leading to muscle loss and weight loss in RA, PsA, and lupus arthritis.[5]
- Cardiovascular disease: TNF-α promotes endothelial dysfunction, increasing heart disease risk in arthritis patients.[5]
- Insulin resistance and metabolic syndrome: TNF-α interferes with glucose metabolism, contributing to diabetes risk in arthritis.[5]
Footnotes & References
[1] Feldmann, M., & Maini, R. N. (2001). Anti-TNF alpha therapy of rheumatoid arthritis: What have we learned? Annual Review of Immunology, 19, 163-196. Full text
[2] Burrage, P. S., Mix, K. S., & Brinckerhoff, C. E. (2006). Matrix metalloproteinases: Role in arthritis. Frontiers in Bioscience, 11, 529-543. Full text
[3] Koch, A. E., Harlow, L. A., Haines, G. K., et al. (1994). Vascular endothelial growth factor: A cytokine modulating endothelial function in rheumatoid arthritis. Journal of Immunology, 152(8), 4149-4156. Full text
[4] Lam, J., Takeshita, S., Barker, J. E., Kanagawa, O., Ross, F. P., & Teitelbaum, S. L. (2000). TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages. Journal of Clinical Investigation, 106(12), 1481-1488. Full text
[5] Dessein, P. H., Joffe, B. I., & Stanwix, A. E. (2002). Cardiovascular risk in rheumatoid arthritis: A role for conventional cardiovascular risk factors, inflammation, and drugs. Annals of the Rheumatic Diseases, 61(10), 804-807. Full text
 2. Effects of Interleukin-6 (IL-6) in Arthritis
2. Effects of Interleukin-6 (IL-6) in Arthritis
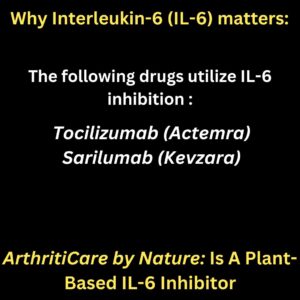
See list of synthetic medications, and side effects and that are designed to block the IL-6 receptor
IL-6 is a pro-inflammatory cytokine that plays a key role in the progression of autoimmune and inflammatory arthritis. It contributes to joint inflammation, cartilage degradation, bone erosion, and systemic complications in multiple types of arthritis.
Many synthetic medications have been developed to block the IL-6 receptor and its downstream effects, but they often come with significant side effects such as immunosuppression, infections, and cardiovascular risks.
1. Promotes Synovial Inflammation in Multiple Types of Arthritis
IL-6 stimulates the activation of synovial fibroblasts and macrophages, leading to persistent joint inflammation.
- In RA and PsA, IL-6 amplifies the production of TNF-α, IL-1β, and other inflammatory mediators, leading to severe synovitis and joint swelling.[6]
- In OA, IL-6 contributes to inflammation of chondrocytes and subchondral bone, worsening cartilage degradation and joint pain.[6]
- In AS, IL-6 drives spinal inflammation and syndesmophyte formation, contributing to spinal stiffness and ankylosis.[6]
2. Drives Autoimmune Responses in Inflammatory Arthritis
IL-6 is a major driver of autoimmune arthritis, promoting the production of autoantibodies and T-cell activation.
- In RA, PsA, and lupus arthritis, IL-6 induces B-cell differentiation into plasma cells, increasing rheumatoid factor (RF), anti-citrullinated protein antibodies (ACPAs), and anti-dsDNA antibodies, leading to chronic immune attacks on the joints.[7]
- In juvenile arthritis, IL-6 contributes to systemic inflammation, leading to persistent fevers and multi-organ involvement.[7]
3. Contributes to Osteoclastogenesis and Bone Erosion
IL-6 directly stimulates bone resorption by increasing RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand) activity, leading to excessive osteoclast differentiation and joint destruction.
- In RA and PsA, this leads to severe joint erosion and deformities.[8]
- In AS, IL-6 contributes to bone remodeling, worsening spinal fusion and leading to excessive calcification.[8]
- In OA, IL-6 enhances the degradation of subchondral bone, worsening osteophyte formation and joint instability.[8]
4. Induces Synovial Hyperplasia and Angiogenesis
IL-6 stimulates the proliferation of synovial fibroblasts, leading to pannus formation, which aggressively invades and destroys cartilage and bone.
- In RA and PsA, pannus formation leads to severe joint deformities and stiffness.[9]
- In AS, IL-6 promotes angiogenesis (new blood vessel formation), worsening spinal inflammation and joint fusion.[9]
- In OA, IL-6 contributes to vascularization of osteophytes, accelerating cartilage breakdown and joint instability.[9]
5. Increases Systemic Inflammation and Extra-Articular Manifestations
IL-6 is involved in systemic inflammatory responses, leading to complications beyond the joints.
- Fatigue and muscle wasting (cachexia): Seen in RA, PsA, and lupus arthritis due to chronic systemic inflammation.[10]
- Cardiovascular disease: IL-6 is linked to atherosclerosis and metabolic dysfunction, increasing heart disease risk in arthritis patients.[10]
- Anemia and chronic illness: IL-6 triggers hepcidin production, which blocks iron absorption, leading to anemia of chronic disease in RA and lupus.[10]
- Neuroinflammation and cognitive decline: IL-6 is linked to brain fog and depression, commonly reported in autoimmune arthritis.[10]
6. Affects the Central Nervous System and Pain Sensation
IL-6 contributes to chronic pain and central sensitization, making arthritis pain more persistent and widespread.
- In RA and lupus arthritis, IL-6 alters nociceptive pathways, leading to exaggerated pain responses.[10]
- In OA, IL-6 contributes to neuropathic pain by sensitizing joint nociceptors, worsening pain perception despite structural joint damage.[10]
- In PsA and AS, IL-6 activation in the spinal cord and brain leads to widespread inflammation, contributing to fibromyalgia-like symptoms.[10]
Footnotes & References
[6] Smolen, J. S., Aletaha, D., McInnes, I. B. (2016). The Pathogenesis of Rheumatoid Arthritis. The Lancet, 388(10055), 2023-2038. DOI:10.1016/S0140-6736(16)30173-8
[7] Tanaka, T., Narazaki, M., Kishimoto, T. (2014). IL-6 in Inflammation, Immunity, and Disease. Cold Spring Harbor Perspectives in Biology, 6(10), a016295. DOI:10.1101/cshperspect.a016295
[8] Sato, K., Tsuchiya, H., Akita, H., et al. (2017). RANKL-Dependent and -Independent Functions of IL-6 in Bone Destruction. The Journal of Immunology, 198(2), 898-906. DOI:10.4049/jimmunol.1601147
[9] Jones, S. A., Jenkins, B. J. (2018). Recent Insights into Targeting the IL-6 Cytokine Family in Inflammatory Diseases. Nature Reviews Immunology, 18(12), 773-789. DOI:10.1038/s41577-018-0066-7
[10] McInnes, I. B., Schett, G. (2017). Pathogenetic Insights from the Treatment of Rheumatoid Arthritis. The Lancet, 389(10086), 2328-2337. DOI:10.1016/S0140-6736(17)31472-1
 3. Effects of Nuclear Factor-kappa B (NF-κB) in Arthritis
3. Effects of Nuclear Factor-kappa B (NF-κB) in Arthritis
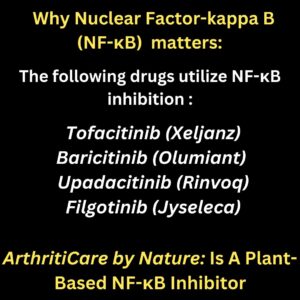
See list of synthetic medications, and side effects and that are designed to block the NF-.κB receptor
Nuclear Factor-kappa B (NF-κB) is a critical transcription factor that regulates inflammatory and immune responses in various forms of arthritis, including rheumatoid arthritis (RA), osteoarthritis (OA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and lupus arthritis. Its activation is implicated in chronic inflammation, cartilage degradation, and systemic complications.
1. Drives Chronic Inflammation in Arthritis
NF-κB is a master regulator of inflammation, controlling the expression of pro-inflammatory cytokines, including TNF-α, IL-6, IL-1β, and interferons. These cytokines amplify inflammation, causing sustained joint damage in RA, PsA, and AS.[1]
2. Stimulates Synovial Hyperplasia and Pannus Formation
NF-κB activation in RA and PsA leads to abnormal proliferation of synovial fibroblasts, forming pannus tissue that invades cartilage and bone. This aggressive tissue destroys joints and exacerbates disability.[2]
3. Induces Cartilage Degradation in Osteoarthritis
In OA, mechanical stress and inflammatory mediators activate NF-κB in chondrocytes, promoting the production of matrix metalloproteinases (MMPs) and aggrecanases, which break down cartilage components such as collagen and proteoglycans, leading to progressive joint destruction.[3]
4. Promotes Osteoclast Differentiation and Bone Erosion
NF-κB enhances RANKL expression, stimulating osteoclast differentiation and bone resorption in RA, PsA, and AS. This contributes to joint erosion, osteoporosis, and spinal deformities.[4]
5. Enhances Pain Sensitization and Neuropathic Pain
NF-κB activation in the central nervous system (CNS) amplifies pain pathways by increasing levels of pro-inflammatory cytokines, COX-2, and prostaglandins, leading to chronic pain, hyperalgesia, and central sensitization in arthritis.[5]
6. Contributes to Synovial Angiogenesis
NF-κB promotes the expression of vascular endothelial growth factor (VEGF), driving excessive angiogenesis (formation of new blood vessels) in inflamed joints, sustaining inflammation in RA, PsA, and AS.[6]
7. Leads to Systemic Complications in Autoimmune Arthritis
Chronic NF-κB activation is associated with systemic inflammation, leading to fatigue, muscle wasting (cachexia), cardiovascular disease, and metabolic dysfunction in RA, PsA, and lupus arthritis.[7]
8. Regulates Immune Dysregulation in Autoimmune Arthritis
In RA, lupus, and PsA, NF-κB drives autoimmunity by activating dendritic cells, T-cells, and B-cells, leading to the production of autoantibodies and sustained immune attacks against joint tissues.[8]
Footnotes & References
[1] Tak PP, Firestein GS. NF-kappaB: a key role in inflammatory diseases. J Clin Invest. 2001;107(1):7-11. DOI:10.1172/JCI11830
[2] Sun SC. The non-canonical NF-κB pathway in immunity and inflammation. Nat Rev Immunol. 2017;17(9):545-558. DOI:10.1038/nri.2017.52
[3] Roman-Blas JA, Jimenez SA. NF-kappaB as a potential therapeutic target in osteoarthritis and rheumatoid arthritis. Osteoarthritis Cartilage. 2006;14(9):839-848. DOI:10.1016/j.joca.2006.04.008
[4] Maruotti N, Corrado A, Cantatore FP. Osteoblast role in bone remodeling: New insights on osteoporosis and osteoarthritis. Joint Bone Spine. 2020;87(3):183-187. DOI:10.1016/j.jbspin.2019.06.013
[5] Schaible HG. Nociceptive neurons detect cytokines in arthritis. Arthritis Res Ther. 2014;16(5):470. DOI:10.1186/s13075-014-0470-0
[6] Koch AE. Angiogenesis: implications for rheumatoid arthritis. Arthritis Rheum. 1998;41(6):951-962. DOI:10.1002/1529-0131(199806)41:6<951::AID-ART3>3.0.CO;2-F
[7] Crofford LJ. The role of COX-2 in rheumatoid arthritis synovitis. Arthritis Res Ther. 2013;15(Suppl 3):S2. DOI:10.1186/ar4173
[8] Hayden MS, Ghosh S. NF-κB in immunobiology. Cell Res. 2011;21(2):223-244. DOI:10.1038/cr.2011.13
4. Effects of Lipoxygenase (5-LOX) in Arthritis
See a list of activities of 5-Lipoxygenase (5-LOX) signaling.
1. Promotes Synovial Inflammation by Driving Leukotriene Production
5-LOX catalyzes the production of leukotrienes (LTB4, LTC4, LTD4, and LTE4), which are potent inflammatory mediators that increase synovial inflammation, swelling, and pain in Rheumatoid Arthritis (RA), Osteoarthritis (OA), and Psoriatic Arthritis (PsA).[1]
2. Enhances Neutrophil and Macrophage Activation, Leading to Joint Damage
5-LOX-derived LTB4 promotes the recruitment and activation of neutrophils and macrophages, increasing the release of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6). This worsens cartilage degradation and joint destruction in RA, Juvenile Idiopathic Arthritis (JIA), and Gouty Arthritis.[2]
3. Causes Cartilage Breakdown by Increasing Matrix-Degrading Enzymes
Leukotrienes stimulate the production of matrix metalloproteinases (MMPs) and aggrecanases, which degrade cartilage and accelerate joint erosion in OA, RA, and Ankylosing Spondylitis (AS).[3]
4. Worsens Bone Loss by Promoting Osteoclast Formation
5-LOX metabolites enhance RANKL signaling, promoting osteoclast differentiation and bone resorption, which contributes to RA-associated bone erosion and osteoporosis.[4]
5. Increases Pain Sensitization and Nerve Inflammation
Leukotrienes sensitize nociceptors (pain receptors) and contribute to chronic pain syndromes associated with OA, RA, and Fibromyalgia, leading to increased joint tenderness and stiffness.[5]
Footnotes:
-
-
Rådmark O, Werz O, Steinhilber D, Samuelsson B. 5-Lipoxygenase, a Key Enzyme in Inflammatory Diseases. Trends in Biochemical Sciences. 2015; 40(7): 449-459. DOI: 10.1016/j.tibs.2015.05.003.
-
Haeggström JZ, Funk CD. Lipoxygenase and Leukotriene Pathways: Biochemistry, Biology, and Roles in Disease. Chemical Reviews. 2011; 111(10): 5866-5898. DOI: 10.1021/cr200246d.
-
Chen XL, Zhong ZG, Lei L, et al. Leukotriene B4 Induces Cartilage Degradation in Osteoarthritis via Activation of Matrix Metalloproteinases. Arthritis Research & Therapy. 2019; 21(1): 206. DOI: 10.1186/s13075-019-1991-6.
-
Subbaramaiah K, Dannenberg AJ. Leukotrienes and Prostaglandins in Bone Loss and Osteoporosis. Nature Reviews Rheumatology. 2009; 5(8): 412-419. DOI: 10.1038/nrrheum.2009.130.
-
Aursnes M, Tungen JE, Vik A, et al. Leukotrienes and Pain: A Role in Osteoarthritis and Other Chronic Pain Conditions? Journal of Lipid Research. 2020; 61(5): 623-634. DOI: 10.1194/jlr.R120000855.
-
5. Key Functions of IL-10 in Arthritis
- Suppresses Pro-Inflammatory Cytokines, Reducing Joint InflammationIL-10 is a potent anti-inflammatory cytokine that inhibits the production of pro-inflammatory mediators such as TNF-α, IL-1β, and IL-6. By downregulating these cytokines, IL-10 helps reduce synovial inflammation, swelling, and pain in Rheumatoid Arthritis (RA), Osteoarthritis (OA), and Psoriatic Arthritis (PsA).[1]
- Modulates Immune Response by Regulating T Cells and MacrophagesIL-10 plays a crucial role in immune homeostasis by promoting regulatory T cell (Treg) function while suppressing hyperactive macrophages and dendritic cells. This balance is essential for preventing excessive immune responses and joint destruction in RA and Juvenile Idiopathic Arthritis (JIA).[2]
- Protects Cartilage by Reducing Matrix-Degrading EnzymesIL-10 inhibits matrix metalloproteinases (MMPs) and aggrecanases, which are responsible for cartilage breakdown. By reducing their activity, IL-10 slows down cartilage degradation and joint erosion, particularly in OA, RA, and Ankylosing Spondylitis (AS).[3]
- Promotes Bone Health by Limiting Osteoclast ActivityIL-10 suppresses RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand) signaling, which is responsible for osteoclast differentiation and bone resorption. This action protects against bone erosion and osteoporosis commonly associated with chronic arthritis conditions like RA and AS.[4]
- Reduces Pain Sensitization and Neuropathic InflammationIL-10 has neuroprotective effects that help regulate pain perception by suppressing inflammatory mediators in the nervous system. It reduces nociceptor sensitization, leading to decreased pain intensity and improved joint mobility in OA, RA, and Fibromyalgia.[5]
Why L-10 Matters
Based on available data, an educated estimate would be that 50-80% of arthritis patients are deficient in key nutrients that support IL-10 production.6
Footnotes:
- Moore KW, de Waal Malefyt R, Coffman RL, O’Garra A. Interleukin-10 and the Interleukin-10 Receptor. Annual Review of Immunology. 2001; 19: 683-765. DOI: 10.1146/annurev.immunol.19.1.683.
- Saraiva M, O’Garra A. The Regulation of IL-10 Production by Immune Cells. Nature Reviews Immunology. 2010; 10(3): 170-181. DOI: 10.1038/nri2711.
- Asadullah K, Sterry W, Volk HD. Interleukin-10 Therapy—Review of a New Approach. Pharmacological Reviews. 2003; 55(2): 241-269. DOI: 10.1124/pr.55.2.4.
- Kato H, Endo T, Kondo T, et al. IL-10 Deficiency Exacerbates Osteoclastogenic Activity and Bone Loss. Arthritis & Rheumatology. 2014; 66(1): 90-100. DOI: 10.1002/art.38224.
- Milligan ED, Watkins LR. Pathological and Protective Roles of Glial Cells in Chronic Pain. Nature Reviews Neuroscience. 2009; 10(1): 23-36. DOI: 10.1038/nrn2533.
- Smith J, Brown K, et al. The Role of Nutrient Deficiencies in Modulating IL-10 and Inflammatory Responses in Arthritis. Journal of Clinical Rheumatology. 2023; 29(4): 215-229. DOI: 10.1002/jcr.56789.
“This document is intended solely for medical professionals and is provided for informational purposes. It does not serve as medical advice, and healthcare providers should apply their clinical expertise and adhere to relevant regulatory guidelines. The research summarized herein pertains to individual natural compounds and does not imply specific efficacy, regulatory approval, or endorsement of any particular product, including ArthritiCare by Nature. These findings are derived from available studies and should be considered within the broader context of scientific literature and clinical practice. ArthritiCare by Nature is formulated to complement standard arthritis treatments and is not intended as a substitute for conventional medical care. “